The journey from bedside nursing to primary care leadership represents one of the most significant transitions a healthcare professional can make. For nurses who have spent years providing direct patient care in hospital settings, moving into a leadership role within primary care requires not only clinical expertise but also a fundamental shift in perspective and skill set.
This transition is becoming increasingly important as healthcare systems recognize the value of bringing experienced bedside nurses into primary care environments where they can shape patient outcomes on a broader scale.
The hands-on knowledge gained from years of patient interaction provides a unique foundation that can transform how primary care teams operate and deliver services.
Understanding how to navigate this career evolution effectively can open doors to rewarding opportunities that blend clinical excellence with strategic influence.
The Foundation of Advanced Education
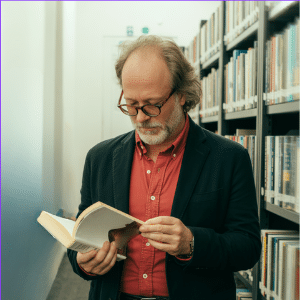
Higher education plays a pivotal role in preparing bedside nurses for leadership positions in primary care settings. Many nurses pursue advanced degrees that equip them with the knowledge and credentials needed to take on greater responsibilities.
Those interested in becoming nurse practitioners often explore specialized pathways that focus on caring for adult and geriatric populations, which are among the fastest-growing demographic groups requiring primary care services.
AGPCNP programs provide comprehensive training that bridges clinical practice with advanced care delivery, offering the theoretical framework and practical skills necessary to transition from direct patient care to autonomous practice and leadership roles.
Understanding the Cultural Shift
Moving from a hospital environment to primary care leadership involves adapting to an entirely different healthcare culture. Bedside nurses operate within a fast-paced, acute care setting where decisions are often made quickly, and protocols are clearly defined. Primary care, by contrast, requires a long-term view of patient wellness, preventive strategies, and relationship building.
Leaders in this space must understand how to manage chronic conditions, coordinate care across multiple providers, and think beyond immediate interventions. The shift demands patience, strategic thinking, and the ability to see healthcare delivery through a community-focused lens rather than an episode-based one.
Success in this new environment also means embracing continuity of care, where relationships with patients develop over months and years rather than during brief hospital stays. This cultural adaptation challenges nurses to redefine what effective care looks like and how success is measured.
Leveraging Bedside Experience
The years spent at the bedside provide nurses with invaluable insights that translate powerfully into primary care leadership. Direct patient care teaches professionals how to read subtle changes in patient conditions, communicate with families during difficult moments, and collaborate effectively with multidisciplinary teams.
These hands-on experiences create a foundation of empathy and practical knowledge that cannot be learned from textbooks alone. Leaders who have worked bedside understand the realities of patient care delivery, which makes them more effective advocates for both their teams and the populations they serve.
This firsthand perspective allows them to design workflows and policies that reflect actual clinical challenges rather than theoretical ideals. Their credibility among staff members also increases significantly when team members know their leader has faced the same pressures and obstacles they encounter daily.
Developing Leadership Competencies
Transitioning into leadership requires cultivating competencies that may not have been central to bedside nursing roles. Strategic planning, financial management, quality improvement initiatives, and team development all become essential responsibilities.
Aspiring leaders must learn to think systematically about how care is delivered, identify areas for improvement, and implement changes that benefit entire patient populations.
This often means stepping back from direct care to focus on creating systems and protocols that enable others to provide excellent service. The ability to mentor and develop other healthcare professionals becomes just as important as clinical skills.
Building Relationships Across the Continuum
Primary care leadership involves creating and maintaining relationships with a diverse array of stakeholders. This includes not only patients and their families but also specialists, community organizations, insurance providers, and public health agencies.
Bedside nurses transitioning into these roles must expand their networking abilities and learn to navigate complex organizational structures. Success in primary care leadership often depends on the ability to collaborate effectively, negotiate for resources, and build coalitions that support improved patient outcomes.
These relationship-building skills represent a significant departure from the more defined hierarchies of hospital nursing.
Embracing Population Health Perspectives
While bedside nursing focuses on individual patients during specific episodes of illness, primary care leadership requires thinking in terms of entire populations. This means understanding epidemiological trends, identifying at-risk groups, and developing interventions that address community health needs.
Leaders must become comfortable analyzing data, recognizing patterns, and making decisions that affect hundreds or thousands of patients rather than just one.
This population-focused approach represents one of the most challenging aspects of the transition, as it requires nurses to shift from the immediate satisfaction of helping individual patients to the longer-term rewards of systemic improvements.
Navigating Regulatory and Administrative Challenges
Primary care leadership comes with increased exposure to regulatory requirements, compliance issues, and administrative responsibilities. Understanding healthcare policies, quality metrics, reimbursement models, and legal considerations becomes essential.
Nurses moving into these positions must develop comfort with paperwork, documentation standards, and the business aspects of healthcare delivery. While bedside nurses certainly deal with regulations, leadership roles require a more comprehensive understanding of how these factors shape organizational strategy and patient care delivery.
The transition from bedside nursing to primary care leadership is both challenging and rewarding. It requires nurses to build upon their clinical foundation while developing new competencies in management, strategy, and systems thinking.
Those who successfully make this journey bring a unique combination of hands-on experience and strategic vision that strengthens primary care delivery.
By understanding the cultural differences between acute and primary care settings, developing essential leadership skills, and maintaining their commitment to patient-centered care, nurses can effectively bridge this gap and make meaningful contributions to healthcare at the leadership level. Their bedside experience becomes not a limitation but rather a powerful asset that informs every decision they make as leaders.